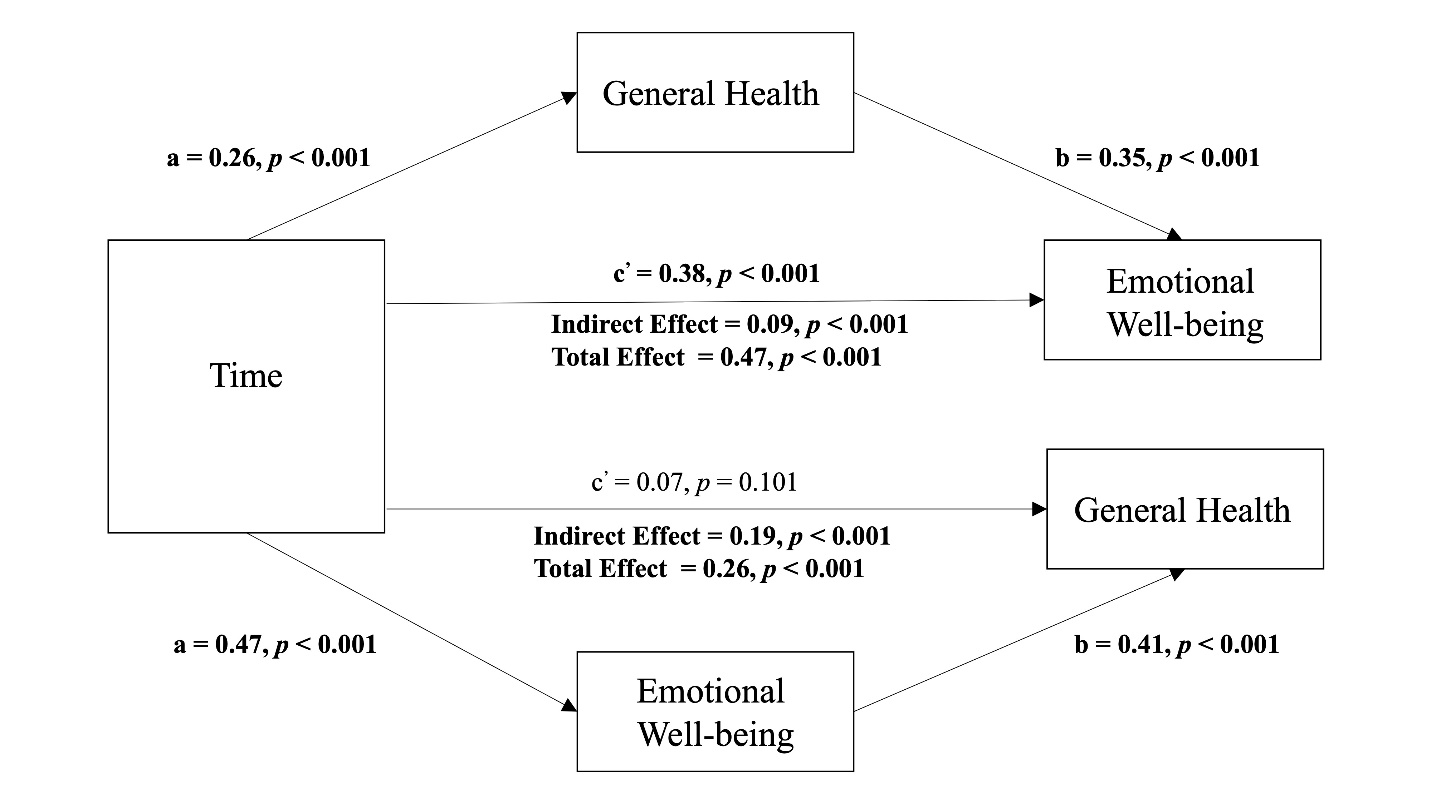
Figure 1. Mediating effect of perceived emotional well-being and general health after an online health coaching intervention.
Note: Mediator variable was collected at the 2-week follow-up and the outcome variable was collected at 4-week follow-up
Associations of an Online Health Coaching Intervention with Movement Behaviors and Perceived Health: A Mediation Analysis
Lingyi Fu1, Ryan D. Burns1, Yuhuan Xie1, Julie E. Lucero1, Timothy A. Brusseau1, and Yang Bai1
1 Department of Health and Kinesiology, University of Utah, USA
Abstract
The purpose of this study was to examine the associations of an online coaching intervention that included goal setting with movement behaviors and perceived general health (GH) and emotional wellbeing (EW) in college students. Participants were college students from a university within the western United States (N=257; 57.2% female). Participants met with health coaches in an online setting for one hour and goals were set for physical activity (PA) and/or sleep duration. PA, sleep duration, and perceptions of GH and EW were collected at baseline and at 2- and 4-weeks after the coaching session within a single arm research design. Mediation analyses determined the indirect effect (IE) of each movement behavior both after the health coaching session and after goal setting on the GH and EW outcomes in addition to the bidirectional association between GH and EW. No movement behavior positively mediated the associations with GH or EW after the health coaching session or after goal setting, although after goal setting PA and weeknight sleep at 2-weeks associated with GH at 4-weeks (b=0.16–0.39, p<0.01) and associated with EW at 4-weeks (b=0.22–0.25, p<0.01). EW mediated the associations of the health coaching session on GH (IE=0.19, p<0.001) and GH mediated the association of the health coaching session on emotional wellbeing (IE=0.09, p<0.001). In conclusion, movement behaviors correlated with GH and EW, but no positive mediating associations were observed. After the health coaching session, EW mediated the association with GH and vice-versa, suggesting a bidirectional association between the two health perceptions.
Keywords: exercise, mental health, mentoring, sleep, young adult
College students are typically within a stage of lifespan development when health habits become increasingly malleable as the transition from secondary school into university comes with challenges to adopt and/or sustain a healthy lifestyle (Arnett, 2000; Sawyer et al., 2018; The Lancet, 2022). Studies have shown that college students are typically inactive and have unhealthy sleep behaviors, which increases risk for cardiometabolic disease and lowers psychological wellbeing (Deliens et al., 2015; Bodziony & Stetson, 2022; Wickham et al., 2020; Wunsch et al., 2017). Although many behaviors may associate with health and wellbeing, examining the behaviors that comprise the “24-hour movement framework”, including physical activity (PA) and sleep duration, is recommended not only because of their compositional nature but also because each behavior may uniquely correlate with health and wellness outcomes (Rosenberger et al., 2019; Rollo et al., 2020; Burns, Bai, et al., 2020).
Various studies have emphasized the positive association between PA, wellbeing, and quality of life, underscoring the importance of promoting PA in college students (Doré et al., 2020; Zhang et al., 2022; Bai et al., 2022). However, the associations between PA and wellbeing may be bidirectional and confounded by other behaviors within the 24-hour framework, such as sleep (Bai et al., 2022; Burns, Bilic, et al., 2023). Longer durations of sleep have been shown to regulate mood and improve quality of life in young people (Kudrnáčová & Kudrnáč, 2023; Scott et al., 2021; Pilcher & Ott, 1998). Some studies have shown that sleep duration is a stronger determinant than PA in regulating mood states (Wunsch et al., 2017; Burns, Bai, et al., 2020; Burns, Bilic, et al., 2023). Therefore, interventions aiming to increase PA and increase the quantity of sleep may have additive benefits for enhancing wellbeing and quality of life (García-Hermoso et al., 2022).
Perceptions of one’s own general health (GH) and emotional wellbeing (EW) are determinants of overall quality-of-life (Menec et al., 1999; Zahrt & Crum, 2017; Foottit & Anderson, 2012; Riediger et al., 2019). Self-reported health and wellbeing has correlated with measured physical and mental health outcomes and longitudinally correlated with mortality rates (Menec et al., 1999; Zahrt & Crum, 2017; Foottit & Anderson, 2012; Riediger et al., 2019). Methods for improving perceptions of GH and EW in college students is relatively sparse. However, goal setting is one approach that can be used to improve both GH and EW in young people (Hanley et al., 2022). The process of goal setting involves the identification of specific behaviors that require adjustment and facilitate healthy habits (Schweitzer et al., 2016). This can include identifying and removing barriers that may preclude reaching goals (Schweitzer et al., 2016). Indeed, goal setting simultaneously focuses on skill development that can facilitate behavior adjustment and the removal of barriers (Bailey, 2017). To instill positive behavioral outcomes and successful goal setting strategies, the incorporation the use of the S.M.A.R.T (Specific, Measurable, Attainable, Realistic, Time-oriented) criteria for goals has been recommended (Bailey, 2017; Pearson, 2012). Research has demonstrated that goal setting interventions using the S.M.A.R.T. approach can produce an increase in PA and longer sleep durations (Bilic et al., 2023).
Recognizing the significance of facilitating health behaviors in college students, this paper aims to fill existing research gaps by determining the extent to which movement behaviors mediate the associations with perceived GH and EW after a brief online health coaching session that involved goal setting. It is currently unclear if PA and sleep can mediate changes in GH and EW after a brief online health coaching session. In a sample of older adolescents, Leahy et al. (2023) found that a high intensity PA intervention improved perceived stress; however, this effect was not explained by the mediated effect of sleep-related variables. Using a similar framework, the purpose of this study was to examine the mediating role of PA and sleep on GH and EW in college students after a brief health coaching session using goal setting. The bidirectional association between GH and EW were also examined. It was hypothesized that PA and sleep at 2-weeks post health coaching session and goal setting would mediate changes in GH and EW after 4-weeks relative to baseline behaviors. Because GH and EW are correlated and both contribute to overall quality of life, it was also hypothesized that GH and EW will show positive bidirectional associations with each other after the health coaching session (Menec, 1999; Zahrt & Crum, 2017; Foottit & Anderson, 2012; Riediger et al., 2019; Lins & Carvalho, 2016).
Methods
Participants
Participants were a non-probability sample of undergraduate students enrolled at a large western United States university (N=257; 57.2% female; 38.4% freshman). Participants were recruited using convenience and snowball sampling methods (e.g., flyers, word-of-mouth). Inclusion criteria included being 18 years old or older and enrolled in college courses at the university. There were no stated exclusion criteria to participate in the study. Demographic characteristics reported at baseline were communicated in Table 1. Most of the sample were non-Hispanics (84.0%), White (56.3%), and had mothers whose education was an associate degree or lower (51.8%). All participants provided their oral and written consent to be a part of this study. All procedures were approved by the authors’ Institutional Review Board.
Table 1
Demographic Characteristics of the Sample at Baseline
|
Variable |
Level |
N (%) |
Missing N (%) |
|
Gender |
Female |
139 (57.4) |
15 (5.8% |
|
|
Male |
53 (21.9) |
|
|
|
Non-Binary |
50 (20.7) |
|
|
Status Year |
Freshman |
96 (38.4) |
7 (2.7) |
|
|
Sophomore |
48 (19.2) |
|
|
|
Junior |
60 (24.0) |
|
|
|
Senior |
43 (17.2) |
|
|
|
5th Year |
3 (1.2) |
|
|
Race |
White |
143 (56.3) |
3 (1.2% |
|
|
Non-White Minority |
111 (43.7) |
|
|
Ethnicity |
Non-Hispanic/Latino |
163 (84.0) |
63 (24.5) |
|
|
Hispanic/Latino |
31 (16.0) |
|
|
Maternal Education |
Associates Degree or Lower |
100 (51.8) |
64 (24.9) |
|
|
Bachelor’s Degree and Higher |
93 (48.2) |
|
Procedures
The study took place in two waves, specifically during Fall 2020 and Spring 2021 semesters and a second wave one year later during the Fall 2022 and Spring 2023 semesters. After determining participant eligibility, baseline data were collected followed by the scheduling of the health coach session. Baseline data were collected using an online questionnaire. Within two weeks after baseline data collection participants met with health coaches in a one-on-one online setting using Zoom. The health coaches were peer undergraduate students who were enrolled in a wellness program at the same university.
The health coaching session was one-hour in duration. All participants in this study only had one coaching session. Participants were directed to university websites and resources (e.g., wellness clinics) based on their goals that were set during the health coaching session. Goals were set as part of a one-hour health coaching session that consisted of three parts: (1) a self-administered survey to provide awareness of wellness and substance use behaviors; (2) a wellness consult with health coach to provide feedback on health habits, using positive image messages to increase motivation for change; and (3) goal planning session with the health coach who set S.M.A.R.T. goals within two wellness areas (PA, sleep, diet, stress, substance use). Participants chose to set goals for only two areas out of PA, sleep, diet, stress management, and substance use (including cigarette/tobacco use, vaping, and alcohol consumption). Not all participants set goals for PA and/or sleep. Participants completed a screening survey to determine study eligibility and then obtained contact information to allow for scheduling. Students completed the one-on-one wellness coaching sessions on PA, healthy eating, stress management, sleep, and substance use behaviors on Zoom. Participants’ demographic data along with their behaviors and perceived health and wellness data were collected at baseline before the health coach meeting. At 2-weeks and at 4-weeks post-meeting, participants completed follow-up surveys to examine changes in behavior and their perceived health and wellness. Follow-up GH and EW data were also collected. All data at each timepoint were collected using one questionnaire that was completed online. To mitigate risk of response bias, participants were told to answer questions truthfully and by themselves and that their information would be identified so nobody would know what their responses were.
Mediator Variables
Physical activity. The PA variables were weekly metabolic equivalent minutes (MET-minutes) calculated from the International Physical Activity Questionnaire-short form (IPAQ-short form) questionnaire for Walking, Moderate PA, Vigorous PA, and total PA. Procedures were calculating total MET-min per week were followed. IPAQ has been validated in the adult population for estimating total PA (Lee et al., 2011). IPAQ assessed PA (MET-min) over the previous 7 days.
Sleep. Two questionnaire items asked about how many hours of sleep the participants accrued during both weeknights and weekend nights. Responses ranged from less than 4 hours to 10 or more hours. The two sleep behaviors duration scores for weeknight and weekend sleep were calculated and analyzed separately. The sleep duration items were adapted from the National Youth Risk Behavior Survey (Brener et al., 2002). Sleep duration was assessed over the previous 2 weeks.
Dependent Variables
Both GH and EW are two separate constructs from two scales (out of 8 total scales) of the SF-36. Total scores from the SF-36 are not recommended to be calculated and analyzed due to its multidimensional nature. The intention of the SF-36 is to capture aspects of Health-Related Quality of Life (Lins & Carvalho, 2016).
General health. GH was calculated from 5-items from the validated SF-36 Health Survey Questionnaire (Brazier et al., 1992). The calculated score ranged from 0 to 100 where higher scores indicated a higher perception of GH. The section header stated “The following items ask about your general health and mental health. Please answer as honestly as possible. All information is confidential and will not be shared with anyone outside the study team”. The 5 items asked “In general, would you say your health is:” with a 1=excellent to 5=Poor response, “I seem to get sick a little easier than others” with a 1=Definitely True to 5=Definitely False response, “I am as health as anyone I know” with a 1=Definitely True to 5=Definitely False response, “I expect my health to get worse” with a 1=Definitely True to 5=Definitely False response, and “My health is excellent” with a 1=Definitely True to 5=Definitely False response. The responses were reversed coded and weighted so that high scores represented good perceived general health with final analyzed scores ranging from 0 to 100.
Emotional wellbeing. EW was also calculated from 5-items from the validated SF-36 Health Survey Questionnaire (Brazier, 1992). The calculated score ranged from 0 to 100 where higher scores indicated a higher perceived EW. The section header stated “These questions are about how you feel and how things have been with you during the past 2 weeks. For each question, please give the one answer that comes closest to the way you have been feeling. How much of the time during the past 2 weeks…”. The 5 items asked “Have you been a very nervous person:” with a 1=all of the time to 5=none of the time response, “Have you felt so down in the dumps that nothing could cheer you up?” with a 1=all of the time to 5=none of the time response, “Have you felt calm and peaceful?” with a 1=all of the time to 5=none of the time response, “Have you felt downhearted and blue” with a 1=all of the time to 5=none of the time response, and “Have you been a happy person” with a 1=all of the time to 5=none of the time response. The responses were reversed coded and weighted so that high scores represented higher perceived emotional wellbeing with final analyzed scores ranging from 0 to 100.
Independent Variables
Time was a multinomial variable coded (0, 1, 2) that represented the baseline time-point and the 2nd and 4th-week follow-up, respectively. Goal setting was a binary variable (No, Yes) that was behavior specific and self-reported by the participant. Participants reporting not setting a behavior-specific goal were coded 0 and participants reporting setting a behavior-specific goal were coded 1.
Covariates
Additional categorical covariates included participant sex, status year, race, ethnicity, and maternal education. Specific categories for the demographic covariates were collapsed to obtain a higher group sample size for analysis. This approach was reflected in binary covariates for ethnicity (Non-Hispanic, Hispanic), race (White, Non-White Minority), and maternal education level (associate degree or lower, bachelor’s degree and higher). Maternal education was a proxy for socioeconomic status. To reduce participant burden and limit the number of items on the questionnaire, no additional pertinent covariates were collected such as on- or off-campus living and number of people within the household.
Statistical analysis
Descriptive statistics were reported as means and standard deviations for continuous variables and as counts and percent for categorical variables. Differences among genders were examined using one-way analysis of variance tests with Bonferroni adjustment and with effect sizes calculated using Cohen’s delta (d). Effect sizes were considered small if d<0.20, medium if d=0.50, and large if d >0.80 (Cohen, 1992). Differences among genders on categorical variables were examined using Pearson chi-squared tests. The primary analyses consisted of several mediation models. Parameters of interest were the indirect effects (IEs=a path´b path), direct effects (DEs=c’ path), and total effects (TEs=c path). IEs were the mediated associations from a mediator variable at 2-weeks (M) between the independent variable (X) and outcome at 4-weeks (Y), the DE the was association of the independent variable (X) on a respective outcome (Y) at 4-weeks independent of the mediator variable at 2-weeks (M), and the TE was the total associations that the independent variable (X) had on a respective outcome at 4-weeks (Y; TE»IE+DE). Percent of TE mediated was calculated using: % mediation = (IE/TE)´100.
Three sets of mediation models were examined. One set of mediation models tested the IE of PA or sleep (M) in the association of the binary goal setting variable (X) with GH and EW outcomes (Y). Another set of models tested the IE of PA or sleep (M) in the association of the multinomial time variable (X) with GH and EW outcomes (Y). Time represented duration after the respective health coaching session. The third set of mediation models tested the IE of GH or EW (M) in the association of the multinomial time variable (X) with GH and EW (Y). All mediators were collected at the 2-week follow-up and all outcomes were collected at the 4-week follow-up. Adjusted models were estimated and standardized path coefficients were reported. Adjusted models controlled for status year, sex, ethnicity, race, and maternal education at both the mediator on outcome models. All mediation models also controlled for the interaction between the independent variable (X) and mediator variable (M). The mediation models were conducted using Stata’s “mediate” package and cross-checked using R 4.3.0 Lavaan package (Statacorp, n.d.; Rosseel, 2012). Missing data were inputted using multiple imputation by chained equations across at least 10 imputation models. Alpha level was set at p<0.05 with analyses carried out using both Stata version 18 (Statcorp., College Station, Texas, USA) and R 4.3.0.
Results
Descriptive Statistics
Descriptive statistics for movement behaviors and health outcomes at baseline were reported within Table 2. No differences among genders were observed at baseline for GH (F=0.40, p = 0.68) or for EW (F=1.53, p=0.22). Additionally, no differences among genders were observed for total MET-min (F=0.13, p=0.87) and for total sleep (F=0.40, p=0.68). Females set more PA goals (c2=28.5, p<0.001) and more sleep goals (c2=15.1, p=0.002) than males or participants reporting being non-binary.
Table 2
Descriptive Statistics for the Total Sample at Baseline
|
Variable |
Level |
Total Sample (N=257) |
Females (n=139) |
Males (n=53) |
Non-Binary (n=50) |
|
Total MET-min Per Week |
|
2490 (2650) |
2616 (2910) |
2671 (2005) |
1960 (1210) |
|
Weeknight Sleep (h) |
|
6.7 (1.4) |
6.8 (1.5) |
6.5 (1.1) |
6.3 (1.5) |
|
Weekend Sleep (h) |
|
7.4 (1.9) |
7.4 (1.5) |
7.5 (1.7) |
6.8 (2.6) |
|
Total Sleep (h) |
|
14.2 (2.9) |
14.2 (3.1) |
14.1 (2.2) |
13.0 (3.6) |
|
General Health Score (0–100 range) |
|
62.5 (16.4) |
63.1 (16.0) |
60.8 (18.0) |
62.5 (8.7) |
|
Emotional Wellbeing Score (0–100 range) |
|
43.4 (8.6) |
42.8 (8.5) |
44.7 (8.7) |
50.0 (8.1) |
|
Set Physical Activity Goals |
No |
151 (71.2%) |
70 (62.0%) |
31 (64.6%) |
50 (100%) |
|
|
Yes |
61 (28.8%) |
43 (38.0%) |
17 (35.4%) |
0 (0%) |
|
Set Sleep Goals |
No |
167 (78.8%) |
81 (71.7%) |
36 (75.0%) |
49 (98.0%) |
|
|
Yes |
45 (21.2%) |
32 (28.3%) |
12 (25.0%) |
1 (2.0%) |
Note: Presented as either means and standard deviations or counts and %. No significant differences were observed among genders.
Goal Setting, Movement Behaviors, and Health Perceptions
Mediating associations from the health behaviors (i.e., PA, sleep) between goal setting (i.e., PA goal and sleeping goal) and two health perception outcomes (i.e., GH and EW) were presented in Table 3. Setting a PA goal had a significantly negative TE (path c) on GH (β=-0.28, p<0.001) and EW (β=-0.14, p<0.05) because setting a PA goal negatively associated with Total Met-min (path a) in both GH (β=-0.27, p<0.001) and EW (β=-0.21, p<0.05) models. In turn, total Met-min significantly and positively associated with both GH (β=0.39, p<0.001) and EW (β=0.25, p<0.001) (path b); however, because of the negative a paths goal setting had significant negative IEs (path a´b) on GH (β=-0.11, p<0.001) and EW (β=-0.05, p<0.05).
Setting a sleeping goal positively associated with GH (path c’, β=0.31, p<0.05), indicating that setting a sleeping goal contributed to better GH. Weeknight sleep also positively associated with GH (path b, β=0.17, p<0.01). However, due to the negative association of setting a sleeping goal on weeknight sleep (path a, β=-0.19, p<0.01), the mediating association of weeknight sleep between setting a sleeping goal and GH was negative (β=-0.03, p<0.05).
Table 3
Coefficients from the Mediation Models for Goal Setting Associating with Health Perceptions
|
Outcome Variable |
Paths/Effects |
Mediator Variable |
||
|
Total MET-min |
Weeknight Sleep |
Weekend Sleep |
||
|
General Health |
a |
-0.27*** |
-0.19** |
-0.25*** |
|
|
b |
0.39*** |
0.17** |
-0.05 |
|
|
c’ (Direct Effect) |
-0.17** |
0.13* |
0.18** |
|
|
a ´ b (Indirect Effect) |
-0.11*** |
-0.03* |
0.01 |
|
|
c (Total Effect) |
-0.28*** |
0.10 |
0.20** |
|
|
|
|
|
|
|
Emotional well-being |
a |
-0.21*** |
-0.13* |
-0.18* |
|
|
b |
0.25*** |
0.22*** |
-0.03 |
|
|
c’ (Direct Effect) |
-0.09 |
0.08 |
0.00 |
|
|
a ´ b (Indirect Effect) |
-0.05* |
-0.03 |
0.00 |
|
|
c (Total Effect) |
-0.14* |
0.05 |
0.01 |
Note: Coefficients are all standardized; bold denotes statistical significance, * p < 0.05, ** p < 0.01, *** p < 0.001.
Health Coaching, Movement Behaviors, and Health Perceptions
Mediating associations from movement behaviors between the health coaching session itself and the health perceptions outcomes were reported in Table 4. The health coaching session showed directly positive association with GH and EW (path c’, β=0.11–0.44, p<0.01). Total MET-min significantly mediated the association between the health coaching session and health perceptions. Total MET-min negatively mediated the association between time and GH (β=-0.01, p<0.05) and the association between time and EW (β=-0.01, p<0.05), indicating that health coaching associated with lower health perceptions through total Met-min. This was because health coaching associated with lower total Met-min (path a). Weeknight and weekend sleep) did not mediate the association between time and health perceptions (p>0.05).
Table 4
Coefficients from the Mediation Models for Health Coaching Associating with Health Perceptions
|
Outcome Variable |
Paths/Effects |
Mediator Variable |
||
|
Total MET-min |
Weeknight Sleep |
Weekend Sleep |
||
|
General Health |
a |
-0.11* |
0.09* |
-0.08 |
|
|
b |
0.16** |
0.085 |
0.04 |
|
|
c’ (Direct Effect) |
0.25*** |
0.21*** |
0.17*** |
|
|
a ´ b (Indirect Effect) |
-0.01* |
0.008 |
-0.00 |
|
|
c (Total Effect) |
0.23*** |
0.22*** |
0.16*** |
|
|
|
|
|
|
|
Emotional Wellbeing |
a |
-0.11** |
0.11* |
0.03 |
|
|
b |
0.11** |
-0.007 |
0.08* |
|
|
c’ (Direct Effect) |
0.41*** |
0.44*** |
0.38*** |
|
|
a ´ b (Indirect Effect) |
-0.01* |
-0.001 |
0.00 |
|
|
c (Total Effect) |
0.40*** |
0.44*** |
0.39*** |
Note: Paths / Effects are all standardized; bold denotes statistical significance, * p < 0.05, ** p < 0.01, *** p < 0.001.
Bidirectional Associations Between Health Perceptions
Figure 1 shows the mediation models, considering EW as the mediator and GH as the outcome, and vice-versa. The health coaching session did not directly associate with GH (β=0.07, p>0.05), but indirectly associated with GH through EW (IE=0.19, p<0.001). Conversely, when GH was the mediator and EW the outcome, the health coaching session positively associated with EW (β=0.38, p<0.001). Moreover, GH positively mediated the association between time and EW (IE=0.09, p<0.001).
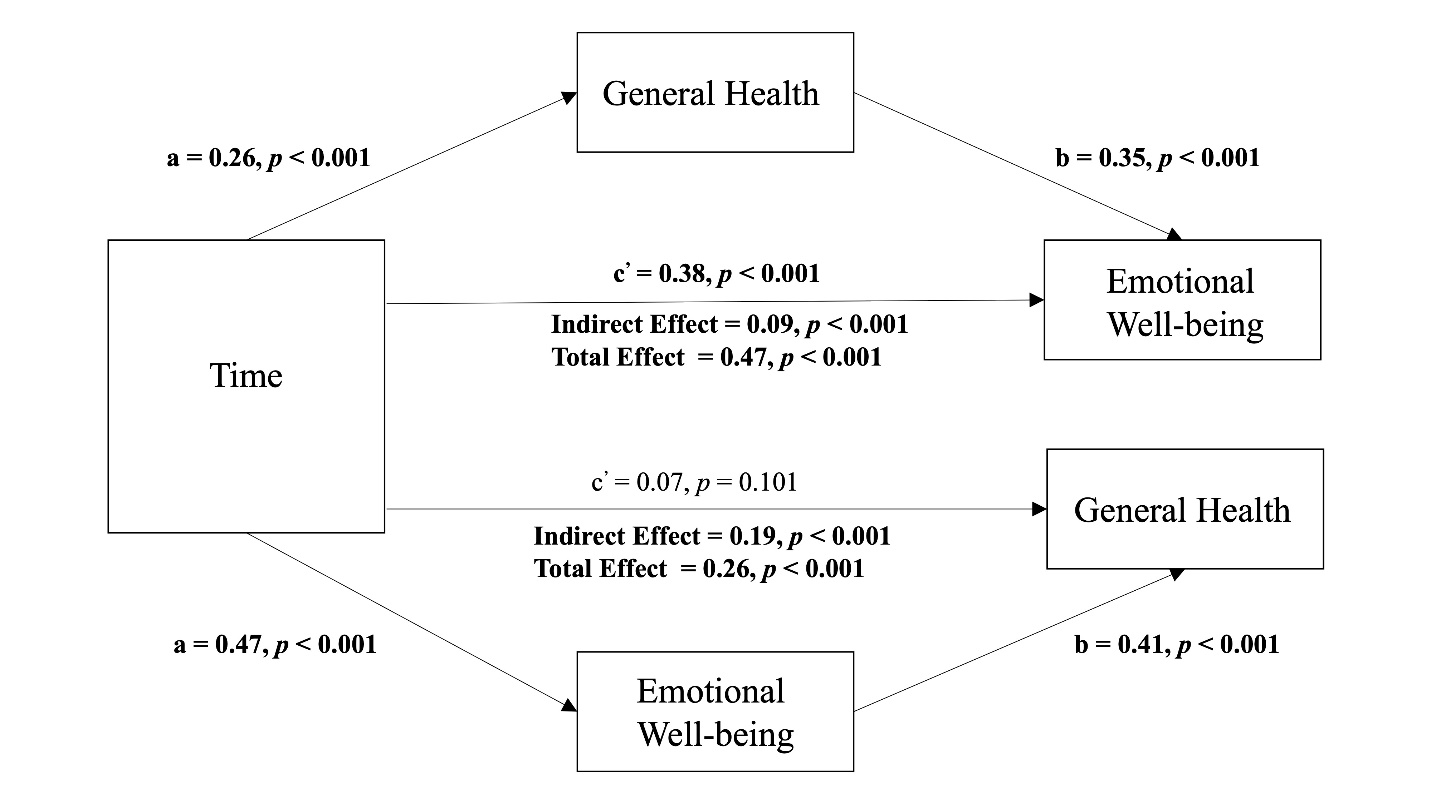
Figure 1. Mediating effect of perceived emotional well-being and general health after an online health coaching intervention.
Note: Mediator variable was collected at the 2-week follow-up and the outcome variable was collected at 4-week follow-up
Discussion
The purpose of this study was to examine the mediating associations of PA and sleep duration on perceptions of GH and EW after an online health coaching intervention in young adults. The results indicated that PA negatively mediated the associations of the health coaching session on health perceptions, although movement behaviors (PA, sleep) at the 2-week follow-up positively associated with self-reported GH and EW at the 4-week follow-up. Additionally, GH and EW mediated each other during the intervention, suggesting a bidirectional association between health perceptions after the health coaching session. An interpretation of these findings has been provided.
A salient finding was that movement behaviors did not positively mediate the association of the health coaching intervention on GH and EW outcomes. In fact, PA (total MET-min) negatively mediated the association between the health coaching intervention and health perceptions. Goals were set for only two health behaviors during the health coach session and PA was the behavior that this sample of young adults set the most goals for (28.7%), followed by setting sleep goals (21.8%). However, at the 2-week follow-up, those who set PA goals had significantly lower total MET-min at follow-up than those who did not set goals. Explanations for this finding using the transtheoretical model of behavior change is that those who set goals were possibly still in the contemplation or preparation stages of behavior change and action for behavior change had not yet occurred (Prochaska & Velicer, 1997; Marcus & Simkin, 1994). Because action on improving PA did not occur, MET-min at 2-week follow-up showed negative mediation with GH and EW outcomes. Similar explanation could be used for sleep duration. Sleep and PA are both time-use behaviors and variation in one behavior is most likely to be associated with variation in the other (Wang et al., 2023; Tremblay et al., 2016). The sleep mediation model showed that those that set sleep goals associated with shorter durations of sleep at 2-weeks. Despite these mediation findings, movement behaviors at 2-weeks did positively associate with health perceptions at 4-weeks. Specifically, higher PA and higher durations of sleep at 2-weeks associated with better GH and EW at 4-weeks. This suggested that perceived health at the 4-week follow-up may have been influenced by movement behaviors at the preceding timepoint, but this association was not initiated by the health coaching intervention and/or by goal setting.
Additional interpretations for participants being stagnant within pre-action stages (e.g., contemplation or preparation) of behavior change is that 2-weeks was not enough time to move into the action stage of behavior change after one brief health coaching session, and/or that setting goals during one coaching session yielded a weak response for behavior change to occur (Bailey, 2017; Marcus & Simkin, 1994). The cycle of goal-setting theory suggests that may be both moderators and specific mechanisms before improvements are realized after setting goals (Bates et al., 2023). These included the mechanisms of attention, effort, and persistence in addition to the moderators of resources, self-efficacy, commitment, and cognitive ability. These mechanisms and moderators can vary significantly at the individual level and can affect the time lag between setting a specific goal, or health coaching in general, and action for behavior change to occur. It is likely that more than one health coaching session is needed to elicit change in behavior with the addition of consistent indication and tracking of specific goals. This could be well executed perhaps using digital methods such as personalized emails and text messages. These methods were not examined in this study but could be addressed in future work. Despite the lack of positive mediation, the health coaching intervention still associated with improvements in GH and EW at 4-weeks, independent of goal setting or positive changes in movement behavior.
When examining the reciprocal mediated associations of GH and EW after the health coaching intervention, the results indicated that both GH and EW at 2-weeks were significant mediator variables when the other was the outcome at 4-weeks, suggesting a potential bidirectional association between GH and EW. Positive affect may have manifested from participants by merely engaging in a health coaching intervention, an association independent of behavior change. Meeting with a health coach or the act of setting goals itself may have elicited support and feelings of connectedness that improved perceptions of GH and EW and possibly overall mental health after the health coach session (Butterworth et al., 2006; Yan et al., 2023). Past research has shown that participating in health programs with peers can yield positive mental health outcomes through mechanisms of social support and connectedness (Aschbrenner et al., 2016). These types of social networks may be even more important for young people due to their continuing brain development within highly changing social environments (Blakemore, 2012; Matud et al., 2020; Mendonça, 2014). During COVID-19, it was shown that school connectedness played an important role in mental health in adolescents, independent of health behaviors, a finding that could be generalized to college students in university settings (Burns & Armstrong, 2022; Hertz et al., 2022). GH an EW are closely correlated and improvements in one perception can lead to improvement in the other after a health coaching intervention and it is this bidirectional association that may provide a mechanism for improvement of these variables at 4-weeks independent from positive changes in behavior.
Strengths of this study included use of panel data derived from an online health coaching intervention delivered to a relatively racially diverse sample of young adults. The mediation analyses controlled for many covariates including demographic covariates and the interaction between the independent variable and mediator variable, which improved the internal validity of the observed results. Limitations to this study included the use of self-report assessments that increased the risk of response bias. Selection bias may have confounded the study’s findings, especially because of the lack of specific exclusion criteria. Participants were a sample of young adults from one US university. It is questionable if the results generalize to other populations of young adults. The results do not generalize to younger or older age groups. Follow-up times were 2-weeks and 4-weeks post health coaching session; therefore, it is unknown whether the effects of the health coaching intervention were sustained after 4-weeks. There was no control or comparison groups to examine the intervention’s effects; therefore, observed relationships should be characterized as associations and no causal inferences can be made. As stated previously, social networks may have confounded the results; however, no variables related to social networks were collected and analyzed in this study. Finally, age, gender, and socioeconomic status could be effect modifiers but were not tested as such.
In conclusion, the 24-hour activity profile behaviors of PA and sleep were not positive mediators on GH and EW after a health coaching intervention. Negative mediation was observed using PA due to sustained lower PA after the health coaching session involving goal setting; suggesting that merely setting PA goals for these behaviors did not translate to actual behavior change and improvement at follow-up. Interestingly, higher levels of PA and better sleep at the 2-week follow-up associated with better perceived GH and EW at the 4-week follow-up. This suggested that perceived health at the 4-week follow-up may have been impacted by movement behaviors at the preceding timepoint, but this association was not initiated by the health coaching and/or by goal setting. Additionally, GH and EW mediated other after the health coaching session, suggesting bidirectional associations between health perceptions that positively predicted each other. In young adults, more than 2-weeks may be needed to observe changes in movement behaviors after a brief online health coaching intervention. However, merely participating in a health coaching intervention may improve positive affect independent of behavioral changes and thus improve one’s own perceptions of GH and EW that may perpetuate after a brief intervention.
Correspondence should be addressed to
Ryan D. Burns
1850 E 250 S Room 237
Salt Lake City, Utah 84112
1-801-695-5035
![]() Ryan
D. Burns: 0000-0002-5933-4633
Ryan
D. Burns: 0000-0002-5933-4633
![]() Julie
E. Lucero: 0000-0003-3874-258X
Julie
E. Lucero: 0000-0003-3874-258X
![]() Timothy
A. Brusseau: 0000-0002-8234-3546
Timothy
A. Brusseau: 0000-0002-8234-3546
Acknowledgements
The authors would like to thank the students who participated in the online health intervention, the wellness coaches, and graduate assistants that aided in the data collection process.
Conflict of Interest
The authors declare no conflicts of interest.
Author Contributions
Conceptualization, L.F., R.D.B., and Y.B.; Methodology, L.F., R.D.B., and Y.B.; Investigation, L.F., R.D.B, Y.X., J.E.L., T.A.B., and Y. B..; Writing – Original Draft, L.F., R.D.B, Y.X., J.E.L., T.A.B., and Y. B.; Writing – Review & Editing, L.F., R.D.B, Y.X., J.E.L., T.A.B., and Y. B., Funding Acquisition, Y.B.; Resources, T.A.B., and Y.B.; Supervision, R.D.B. and Y.B.
Creative Commons License
This work is licensed under a Creative Commons Attribution-Noncommercial 4.0 International License (CC BY-NC 4.0).
Funding
This work was supported by the Salt Lake County Health Department, Salt Lake City, Utah, United States with software support from the University of Utah Clinical and Translational Science Institute under Grant [number UL1TR002538].
References
Arnett, J. J. (2000). Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol. 55(5):469-480.
Aschbrenner, K. A., Mueser, K. T., Naslund, J. A., et al. (2016). Feasibility Study of Increasing Social Support to Enhance a Healthy Lifestyle Intervention for Individuals with Serious Mental Illness. J Soc Social Work Res. 7(2):289-313. doi:10.1086/686486
Bai, Y., Copeland, W. E., Burns, R., et al. (2022). Ecological Momentary Assessment of Physical Activity and Wellness Behaviors in College Students Throughout a School Year: Longitudinal Naturalistic Study. JMIR Public Health Surveill. 8(1):e25375. doi:10.2196/25375
Bailey, R. R. (2017). Goal Setting and Action Planning for Health Behavior Change. Am J Lifestyle Med. 13(6):615-618. doi:10.1177/1559827617729634
Bates, T. C., Enkbat, T., Gray, E., Lee, J., & Zakharim, M. (2023). How to get things done: tight linkage of conscientiousness with twelve mechanisms of Goal Setting Theory. Person Individ Differ. 214:112331. doi:10/1016/j.paid.2023.112331
Bilic, A,. Burns, R. D., Bai, Y., Brusseau, T. A., Lucero, J. E., & King Jensen, J. L. (2023). Preliminary efficacy of a multi-behavioral Zoom-based peer health coaching intervention in young adults: a stepped wedge randomized controlled trial. Cyberpsychol Behav Soc Netw. 26(9):698-705. doi:10.1089/cyber.2022.0365
Blakemore, S. J. (2012). Development of the social brain in adolescence. J R Soc Med. 105(3):111-116. doi:10.1258/jrsm.2011.110221
Bodziony, V. & Stetson, B. (2022). Associations between sleep, physical activity, and emotional well-being in emerging young adults: Implications for college wellness program development. J Am Coll Health. 1-11. doi:10.1080/07448481.2022.2066957
Brazier, J. E., Harper, R., Jones, N. M., et al. (1992). Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 305(6846):160-164. doi:10.1136/bmj.305.6846.160
Brener, N. D., Kann, L., McManus, T., Kinchen, S. A., Sundberg, E. C., & Ross, J.G. (2002). Reliability of the 1999 youth risk behavior survey questionnaire. J Adolesc Health. 31(4):336-342. doi:10.1016/s1054-139x(02)00339-7
Burns, R. D. & Armstrong, J. A. (2022). Associations of connectedness and parental behaviors with adolescent physical activity and mental health during COVID-19: A mediation analysis using the 2021 adolescent behaviors and experiences survey. Prev Med. 164:107299. doi:10.1016/j.ypmed.2022.107299
Burns, R. D., Bai, Y., Pfledderer, C. D., Brusseau, T.A., & Byun, W. (2020). Movement Behaviors and Perceived Loneliness and Sadness within Alaskan Adolescents. Int J Environ Res Public Health. 17(18):6866. doi:10.3390/ijerph17186866
Burns, R. D., Bilic, A., Bai, Y., Brusseau, T. A., Lucero, J. E., & King Jensen, J. L. (2023). Bidirectional associations of physical activity, sleep, and self-reported mental health in young adults participating in an online wellness intervention during the COVID-19 pandemic. Front Public Health. 11:1168702. doi:10.3389/fpubh.2023.1168702
Butterworth, S., Linden, A., McClay, W., & Leo, M.C. (2006). Effect of motivational interviewing-based health coaching on employees’ physical and mental health status. J Occup Health Psychol. 11(4):358-365. Doi:10.1037/1076-8998.11.4.358
Cohen, J. (1992). A power primer. Psychol Bull. 112(1):155-159. Doi:10.1037//0033-2909.112.1.155
Deliens, T., Deforche, B., De Bourdeaudhuij, I., Clarys, P. (2015). Determinants of physical activity and sedentary behaviour in university students: a qualitative study using focus group discussions. BMC Public Health. 15:201. doi:10.1186/s12889-015-1553-4
Doré, I., Sylvester, B., Sabiston, C., et al. (2020). Mechanisms underpinning the association between physical activity and mental health in adolescence: a 6-year study. Int J Behav Nutr Phys Act. 17(1):9. doi:10.1186/s12966-020-0911-5
Foottit, J., Anderson, D. (2012). Associations between perception of wellness and health-related quality of life, comorbidities, modifiable lifestyle factors and demographics in older Australians. Australas J Ageing. 31(1):22-27. doi:10.1111/j.1741-6612.2011.00526.x
García-Hermoso, A., Ezzatvar, Y., Ramírez-Vélez, R., López-Gil, J. F., & Izquierdo, M. (2022). Trajectories of 24-h movement guidelines from middle adolescence to adulthood on depression and suicidal ideation: a 22-year follow-up study. Int J Behav Nutr Phys Act. 19(1):135.doi:10.1186/s12966-022-01367-0
Hanley, T., Prescott, J., & Sefi, A. (2022). The Therapeutic Goals Set by University Students in an Anonymous Web-Based Therapy and Support Setting. Front Psychol. 13:745537. doi:10.3389/fpsyg.2022.745537
Hertz, M. F., Kilmer, G., Verlenden, J., et al. (2022). Adolescent Mental Health, Connectedness, and Mode of School Instruction During COVID-19. J Adolesc Health. 2022;70(1):57-63. doi:10.1016/j.jadohealth.2021.10.02
Kudrnáčová, M. & Kudrnáč, A. (2023). Better sleep, better life? testing the role of sleep on quality of life. PLoS One. 18(3):e0282085. doi:10.1371/journal.pone.0282085
The Lancet. (2022). An age of uncertainty: mental health in young people. Lancet. 400(10352):539. doi:10.1016/S0140-6736(22)01572-0
Leahy, A. A., Diallo, T. M. O., Eather, N., et al. (2023). Mediating effects of sleep on mental health in older adolescents: Findings from the Burn 2 Learn randomized controlled trial. Scand J Med Sci Sports. 33(11):2369-2380. doi:10.1111/sms.14463
Lee, P. H., Macfarlane, D. J., Lam, T. H., & Stewart, S. M. (2011). Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act. 8:115. doi:10.1186/1479-5868-8-115
Lins, L. & Carvalho, F. M. (2016). SF-36 total score as a single measure of health-related quality of life: Scoping review. SAGE Open Med. 4:2050312116671725. doi:10.1177/2050312116671725
Marcus, B. H. & Simkin, L. R. (1994). The transtheoretical model: applications to exercise behavior. Med Sci Sports Exerc. 26(11):1400-1404.
Matud, M. P., Díaz, A., Bethencourt, J. M., & Ibáñez, I. (2020). Stress and psychological distress in emerging adulthood: a gender analysis. J Clin Med. 9:2859. doi:10.3390/jcm9092859
Mendonça, G., Cheng, L. A., Mélo, E. N., de Farias Júnior, J. C. (2014). Physical activity and social support in adolescents: a systematic review. Health Educ Res. 29(5):822-839. doi:10.1093/her/cyu017
Menec, V. H., Chipperfield, J. G., & Perry, R. P. (1999). Self-perceptions of health: a prospective analysis of mortality, control, and health. J Gerontol B Psychol Sci Soc Sci. 54(2):P85-P93. doi:10.1093/geronb/54b.2.p85
Pearson, E. S. (2012). Goal setting as a health behavior change strategy in overweight and obese adults: a systematic literature review examining intervention components. Patient Educ Couns. 87(1):32-42. doi:10.1016/j.pec.2011.07.018
Pilcher, J. J. & Ott, E. S. (1998). The relationships between sleep and measures of health and well-being in college students: a repeated measures approach. Behav Med. 23(4):170-178. doi:10.1080/08964289809596373
Prochaska, J. O. & Velicer, W. F. (1997). The transtheoretical model of health behavior change. Am J Health Promot. 12(1):38-48. doi:10.4278/0890-1171-12.1.38
Riediger, N. D., Bombak, A. E., & Mudryj, A. N. (2019). Health-related behaviours and their relationship with self-rated health among Canadian adults. BMC Public Health. 19(1):960. doi:10.1186/s12889-019-7249-4
Rollo, S., Antsygina, O., & Tremblay, M. S. (2020). The whole day matters: Understanding 24-hour movement guideline adherence and relationships with health indicators across the lifespan. J Sport Health Sci. 9(6):493-510. doi:10.1016/j.jshs.2020.07.004
Rosenberger, M. E., Fulton, J. E., Buman, M. P., et al. (2019). The 24-Hour Activity Cycle: a new paradigm for physical activity. Med Sci Sports Exerc. 51(3):454-464. doi:10.1249/MSS.0000000000001811
Rosseel Y. (2012). Iavaan: An R package for structural equation modeling. Journal Stat Softw. 48:1-36. doi:10.18637/jss.v048.i02
Sawyer, S. M., Azzopardi, P. S., Wickremarathne, D., & Patton, G. C. (2018). The age of adolescence. Lancet Child Adolesc Health. 2(3):223-228. doi:10.1016/S2352-4642(18)30022-1
Schweitzer, A. L., Ross, J. T., Klein, C. J., Lei, K. Y., & Mackey, E. R. (2016). An Electronic Wellness Program to Improve Diet and Exercise in College Students: A Pilot Study. JMIR Res Protoc. 5(1):e29. doi:10.2196/resprot.4855
Scott, A. J., Webb, T. L., Martyn-St James, M., et al. (2021). Improving sleep quality leads to better mental health: A meta-analysis of randomised controlled trials. Sleep Med Rev. 60:101556. doi:10.1016/j.smrv.2021.101556
Statacorp. (n.d.). mediate – Causal mediation analysis. Retrieved September 15, 2023, from https://www.stata.com/manuals/causalmediate.pdf.
Tremblay, M. S., Carson, V., Chaput, J. P., et al. (2016). Canadian 24-Hour movement guidelines for children and youth: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 41(6 Suppl 3):S311-S327. doi:10.1139/apnm-2016-0151
Wang, S., Liang, W., Song, H., et al. (2023). Prospective association between 24-hour movement behaviors and mental health among overweight/obese college students: a compositional data analysis approach. Front Public Health. 11:1203840. doi:10.3389/fpubh.2023.1203840
Wickham, S. R., Amarasekara, N. A., Bartonicek, A., & Conner, T. S. (2020). The big three health behaviors and mental health and well-being among young adults: a cross-sectional investigation of sleep, exercise, and diet. Front Psychol. 11:579205. doi:10.3389/fpsyg.2020.579205
World Health Organization. (2018). Global coordination mechanism on the prevention and control of NCDs: NCD and Youth, 2018. WHO. Available at: http://www.who.int/global-coordination-mecha nism/ncd-themes/ncd-and-youth/ en/2018
Wunsch, K., Kasten, N., & Fuchs, R. (2017). The effect of physical activity on sleep quality, well-being, and affect in academic stress periods. Nat Sci Sleep. 9:117-126. doi:10.2147/NSS.S132078
Yan, Z., Peacock, J., Cohen, J. F. W., et al. (2023). An 8-Week Peer Health Coaching Intervention among College Students: A Pilot Randomized Study. Nutrients. 15(5):1284. Published 2023 Mar 4. doi:10.3390/nu15051284
Zahrt, O. H. & Crum, A. J. (2017). Perceived physical activity and mortality: Evidence from three nationally representative U.S. samples. Health Psychol. 36(11):1017-1025. doi:10.1037/hea0000531
Zhang, Z., He, Z., & Chen, W. (2022). The relationship between physical activity intensity and subjective well-being in college students. J Am Coll Health. 70(4):1241-1246. doi:10.1080/07448481.2020.1790575